美国三名医学科学家和无疆界医生组织分别荣获了2015年拉斯克医学奖。
三名科学家分别是94岁的遗传学家维特金(Evelyn Witkin);
罗格斯大学(New Jersey, nord-est) 退休教授斯蒂芬•约瑟夫•埃利奇(StephenJoseph Elledge);他应该是哈佛大学的教授。
德克萨斯州大学癌症研究中心教授、免疫学家艾利森(James Allison)。
获得2015年的拉斯克医学奖的无国界医生组织在与埃博拉病毒抗争中做出了卓越的贡献。截至2013年超过300人次获得拉斯克奖,其中至少已有81人相继获得过诺贝尔奖,因此被看作诺贝尔奖的“风向标”。2011年拉斯克医学奖获得者屠呦呦,是中国首位获得该奖的中国科学家。
从事肿瘤免疫治疗的科学家詹姆斯•埃里森James Allison。埃里森是德克萨斯大学安德森免疫学学院癌症中心的癌症免疫学家,2014年埃里森曾获得美国国家癌症研究基金会(National Foundation for Cancer Research ,NFCR)第9届圣.乔奇癌症研究创新成就奖。2015年生物和生物化学基础研究领域路易莎·格罗斯·霍维茨奖。
Allison的工作极其重要,是癌症治疗的一个转折点。Allison博士在癌症免疫领域的研究成果帮助医生挽救了无数癌症患者生命,根据他的发现设计的免疫治疗让恶性黑色素瘤患者生存时从不足1年延长到10年,他的研究为肿瘤学发展指明了方向。现在,免疫疗法已深入人心,关于肿瘤免疫的研究彻底扭转了过去人们对治疗癌症的看法。这样的研究就是值得获得诺贝尔医学奖的成果。突出贡献表现在,概念颠覆和扭转,促进了技术和应用。
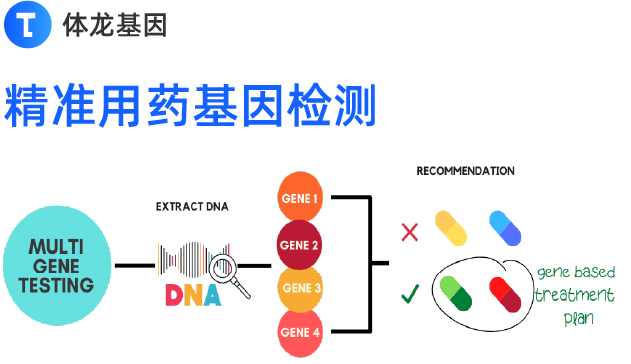
1980年代末,癌症的免疫疗法初见端倪,法国研究者发现在T细胞上有一种叫做CTLA-4的受体。Allison发现该受体会阻止T细胞全力攻击入侵者。1990年代中期,Allison证明,在小鼠中阻断CTLA-4可在小鼠中解除T细胞对肿瘤细胞进行攻击的束缚,从而使肿瘤细胞大幅萎缩。2011年,美国FDA批准伊匹单抗(Yervoy),一种抗CTLA-4抗体用于转移性黑素瘤治疗。2013年,癌症免疫疗法被《科学》杂志评为年度最重要的科学突破。
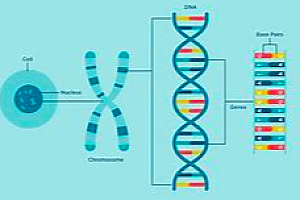
CTLA-4的全称叫做细胞毒性T细胞相关蛋白-4(Cytotoxic T lymphocyte associateprotein-4),它是T细胞表面表达的一类共刺激分子(co-stimulatorymolecule)。与CD28的功能类似,在T细胞激活过程中,CTLA-4能够与APC表面的CD80/CD86特异性结合来激活下游信号。CTLA-4又名CD152,是一种白细胞分化抗原,是T细胞上的一种跨膜受体,与CD28共同享有B7分子配体,而CTLA-4与B7分子结合后诱导T细胞无反应性,参与免疫反应的负调节。基因重组的CTLA-4 Ig可在体内外有效、特异地抑制细胞和体液免疫反应,对移植排斥反应及各种自身免疫性疾病有显著的治疗作用,毒副作用极低,是目前被认为有希望的免疫抑制药物。
拉斯克医学奖,(Lasker MedicalResearch Awards),全称艾伯特·拉斯克奖,是生理学和医学领域除诺贝尔生理学或医学奖外的又一顶级大奖。该奖项始于1946年,是由纽约的阿尔伯特·玛丽·拉斯克基金会设立的,旨在表彰医学领域作出突出贡献的科学家、医生和公共服务人员。拉斯克奖最初分为基础医学奖、临床医学奖和公众服务奖,后又增设特殊贡献奖,前两项专门授予科学家,其得奖者通常会在随后的一年得到诺贝尔奖,该奖项在医学界又素有“诺贝尔奖风向标”之称。拉斯克医学奖也是世界生物医学研究进展的一部编年史。
His newest accolade is designed torecognize researchers whose contributions have improved the clinical treatmentof patients. Allison’s seminal work focuses on a protein called CTLA-4,which reins in T-cell activation in the immune system. By suppressing themolecular brakes that would otherwise block CTLA-4, Allison found he couldunleash the T cells to combat tumors. That discovery helped fuel new cancertreatments including immunotherapy for metastatic melanoma that has been shownto extend patients’ longevity by as much as a decade (medianlife expectancy for metastatic melanoma is under one year).
Another Lasker award, whichhonors basic research, will go to Stephen Elledge and Evelyn Witkin for their work unraveling thefundamentals of how the body detects and corrects for DNA damage. DoctorsWithout Borders will also receive a Lasker Public Service Award for itshumanitarian work responding to Ebola in West Africa.
Allison, chair of the immunologydepartment at the University of Texas M.D. Anderson Cancer Center in Houstonand executive director of its research center on immunotherapy, spokewith Scientific American aboutthe future
inthe mid 1990s you helped pioneer the field by finding that if a key molecularbrake system could be sidelined, then the immune system would be able to moreeffectively kill cancer cells. What makes immunotherapy so different from othercancer treatments?
Traditional cancer therapies are typically drugs thatattack the mutations causing the cancer. That’s a good idea but there are a fewproblems there including the fact that the tumor becomes resistant to the drug.
Whatwe call “checkpoint blockade” therapy – the immunotherapy we’re talking abouthere – differs in a few ways. We get the immune system to attack the process ofcarcinogenesis itself. Checkpoint blockade actually employs T cells to affecttumor cells. T cells detect mutant or foreign peptides on the surface of cellsto give the immune system an idea of what is going on. With lung cancer ormelanoma there are hundreds of thousands of mutations. So with checkpointblockade T cells will recognize new peptides that shouldn’t be there. Then,once you have T cells, unlike with chemotherapy or radiation, there is memory. You have T cells for therest of your life, so if the tumor reoccurs those T cells can mobilizethemselves again against the tumor. The last difference is adaptability. Sinceyour immune system is a dynamic thing, if the tumor changes, the immune systemcan change its response as well.
Beforethe mid 1990s there was still some history with immunotherapy.
Yes,the fact that the immune system could be used to treat cancer was first proposedin 1909 by Paul Ehrlich and he had the idea about antibodies. He thought theimmune system had antibodies that could eliminate tumors. The question was whatantibodies could we use? The reason I think there is so much excitement aboutcheckpoint blockade is it’s relatively easy. You inject an antibody into aperson. And you target the immune system and unleash it and there are manydifferent ways to do it that can be combined. It’s the renaissance ofimmunotherapy. I would say it’s the rebirth of immunotherapy rather than it’snew.
Sometimescancer patients treated with immunotherapy will have their tumors initiallyexpand. That underscores how difficult it is to measure progress duringimmunotherapy. Do you see that as one of the largest challenges in the yearsahead?
Notreally. It caused some concern initially because people thought the tumors weregrowing faster. Now we know it is pseudo-progression. The tumors are actuallyfilling up with T cells, so if you biopsy them you find there are no living tumorcells in there. It’s actually T cells. This did confound the field for a whilebecause with traditional therapies an expanding tumor is a sign of failure. Sowe have to evaluate success differently. There are two ways it’s been dealtwith: one is looking at the tumor again at a different time point. The otherway is to look at overall survival.
Atone point, scientists thought that interferon was going to cure cancer, as weremonoclonal antibodies, for that matter. Do you think unrealistic hopes are mountingfor immunotherapy?
No.I think we are far enough along with it, with over 50,000 patients treated—somewho are 10 years out now—that our hopes are not unrealistic. It’s clear this isnot going to cure every patient, but treatments that include immunotherapy aremore effective than other options. This field is expanding very rapidly. Theimmune system is such a powerful thing that needs to be tightly regulated. Wehave revealed how to take advantage of it to treat cancer.
Doyou think any particular cancers will not be treatable with immunotherapy orwill not have immunotherapy as part of a treatment package to combat them?
Theoretically,since we are not treating the cancer, the cancer doesn’t really matter.
Melanomaand lung cancer, where most of this work has been done, both have a lot ofmutations. They have hundreds of thousands of mutations per cell and it’s themutations the immune system recognizes. When you get to cancers like breast,prostate and kidney, which have smaller numbers of mutations, the drugs aren’tquite as effective. Our job now is to figure out how to make immunotherapyeffective against those tumors with small numbers of mutations. I think theremay be some that don’t respond to [immunotherapy] but I’m pretty optimistic thatwe will be able to deal with a very large number of types of cancer.
Withthe soaring costs of some new drug treatments do you worry that most of theseimmunotherapies will be beyond the financial reach of all but the very rich?
Yes,I do actually. But I should point out there are other drugs, particularly someof the drugs that target the vasculature, that cost $50,000 per year and arebasically given continually after initial treatment. And they really aren’tthat effective. With these checkpoint blockade drugs [this type ofimmunotherapy] there is a pretty high quality of life and patients can quicklyreturn to the workplace. The economic benefit to society with these drugsexceeds the costs. There are still some adverse events with these drugs but it’snothing like that with chemotherapy.
Havingsaid that, these drugs are too expensive. I do worry about the cost being toohigh. I think it’s not going to be possible if you give a combination of two ofthese drugs to charge twice the amount. That’s not possible and it will breakthe bank. I do think the price needs to come down and that it will come downwith more competition with these drugs as more companies develop thesetreatments.
Whatdrew you to science and cancer research in particular?
Whatdrew me to science was just being curious as a kid. I liked to solve problemsand figure out how things work. I had a chemistry set in the garage and myfather supported my interests. I think he wanted me to be a physician but I wasmore interested in science. I was inspired by good teachers and I was luckyenough to be in a summer program after my junior year of high school at theUniversity of Texas at Austin. There I got to do an experiment. It was kind ofa silly thing – identifying how much iron a particular strain of yeast neededto grow optimally but it hooked me on science and lab work.
CancerI became particularly interested in because my mother died from lymphoma when Iwas kid. I saw the effects of the radiation treatment she was receiving. I alsosaw the ravages of the treatment on her brothers who also died from cancer. Oneof her brothers had lung cancer and another had melanoma. I saw personally thetoll that the disease takes. More recently my older brother died frommetastatic prostate cancer. Both me and my other brother had prostate cancer,too, but we caught it quickly with me and I’m fine. It’s had a big impact on myfamily.
Ididn’t specifically go into cancer research. I wanted to see how the immunesystem works. I worked on the problem because I was interested in T cells. It’simportant to not just use your knowledge for the joy of learning and knowingsomething but to help people, too.
Whatsort of advice do you like to give to young scientists?
Scienceis fun but it’s hard work. I think there’s too much pressure now to tell peopleto work on translational science and do things that have immediate clinicalrelevance. I think what people should do is ask important questions infundamental biology and every now and then think about how this impacts humanhealth rather than spend all your time trying to solve a health issue. I thinkthere is still a place for really good fundamental research.
Whatexcites you going forward?
Weknow we can get durable responses lasting a decade or more with a few cancers.I’m optimistic as a field that we can eliminate or at least combat many typesof cancer very soon.
有人提出,在免疫治疗领域,PD-1、Cart-T都是成功的内容,而且名气似乎更大,为什么另外两个没有获奖?
(责任编辑:sgx)